Cigna
Cigna telephone numbers and claim mailing addresses vary by group. Submit electronic claims with payer number 62308.
Information available on the non-secure portion of Cigna's website includes:
Providers are also encouraged to register for secure access to Cigna for Health Care Professionals.Tools on this site allow providers to:
- check claim status
- obtain information about eligibility and benefits
- view and submit precertification requests
- claim editing and bundling procedures
Cigna plan types are OAP and PPO in the following areas:
- Illinois (Carrol, Jo Daviess, Mercer, and Rock Island counties only)
- Iowa
- Nebraska
- South Dakota
The member ID card requires the Midlands Choice logo.
Members with the plan types listed above may also have an "Away From Home" logo on the back of their ID cards. Presence of this logo indicates that the member has in-network access to Midlands Choice providers, whether or not the Midlands Choice logo appears on the card.
Other important information on the backs of ID cards includes:
- customer service telephone numbers
- claim mailing addresses
- precertification telephone numbers and whether precertification is required for inpatient services only, or both inpatient and outpatient services.
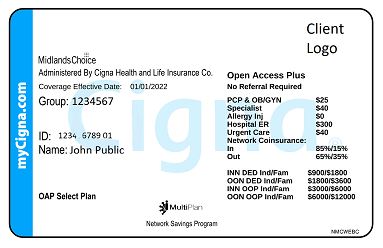 Cigna Sample Card
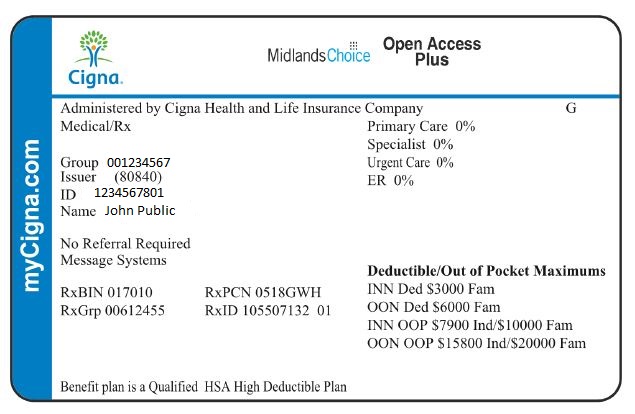
Cigna Sample Card
GWH-Cigna
Submit Great-West Healthcare-Cigna(GWH-Cigna) claims directly to GWH-Cigna at the claims address on the member's ID card: PO Box 188061, Chattanooga, TN 37422-8061. Submit electronic claims with payer number 62308.
GWH-Cigna Sample Card
C/O Cigna Business
Some employers require a higher level of customization and flexibility that aligns with the capabilities of a Third Party Administrator(TPA). Cigna Payer Solutions has relationships with select TPA, Business Process Outsourcers(BPOs) and insurers to offer a breadth of Cigna products that complement the TPA’s administrative and service capabilities.
In these relationships, Cigna Payer Solutions:
- Provides access to our network
- Performs medical management and utilization reviews
- Reprices claims according to our contracted rates and claim logic
- Provides clinical appeals management
TPA's, BPO's and insurers:
- Maintain eligibility
- Administer benefits
- Pay claims for these shared accounts using their own systems and vendors
Cigna administers the contractual relationship with health care professionals to resolve contract language and intent differences.
Additional information:
- ID Cards: ID cards contain the Cigna logo and have the letter "S" on the front of the card to designate that Cigna shares the administration of the plan with a third party.
- Each card includes the paper and electronic claim submission addresses.
- ID cards include the TPS or insurer's telephone number and address(es) for eligibility, benefits, claim status and inquiry.Please contact the TPA with questions on these topics.